Frozen Shoulder - the enigma. Instalment 1
Apr 04, 2019
Frozen shoulder. The enigma. Often referred to as the last remaining mystery in MSK medicine. I think this is overly dramatic. We actually know quite a lot about frozen shoulder (FS) and are slowly unravelling some of the uncertainty surrounding diagnosis and management. Hence, the objective of this review is to dispel some myths and misconceptions regarding FS and clearly articulate what we do know.
Because FS is a LARGE topic, I will break this literature review down into 3 sub-categories. The first will explore the history and subjective examination. The second will outline objective examination and differential diagnosis, and the third will look at management and the future. So for the next 3 months, I will take you on a tour de force of all things frozen shoulder!
Background
Frozen shoulder was first described in the literature by French Pathologist Duplay (1896) and was termed pari-arthrite scapula humerale. Initially thought to be an inflammation of the subacromial bursa causing stiffness and pain of the shoulder complex. Codman (1934) suggested the term Frozen Shoulder (FS) and argued the condition represented a non-calcifying tendonitis of the rotator cuff and was associated with slow onset of symptoms, pain near the insertion of the deltoid, inability to sleep on the affected side, restriction of external rotation and elevation and normal radiological appearance (1). Neviaser (1945) then suggested the term adhesive capsulitis due to the observations of adhesions between the shoulder capsule and the humeral head (2). Summaries of the history and patho-aetiology have been published (3,4). Lewis (2015) suggested the term frozen shoulder contracture syndrome, which should be used with the clinical signs of a FS and when there is evidence of a contraction of the glenohumeral joint capsule (3).
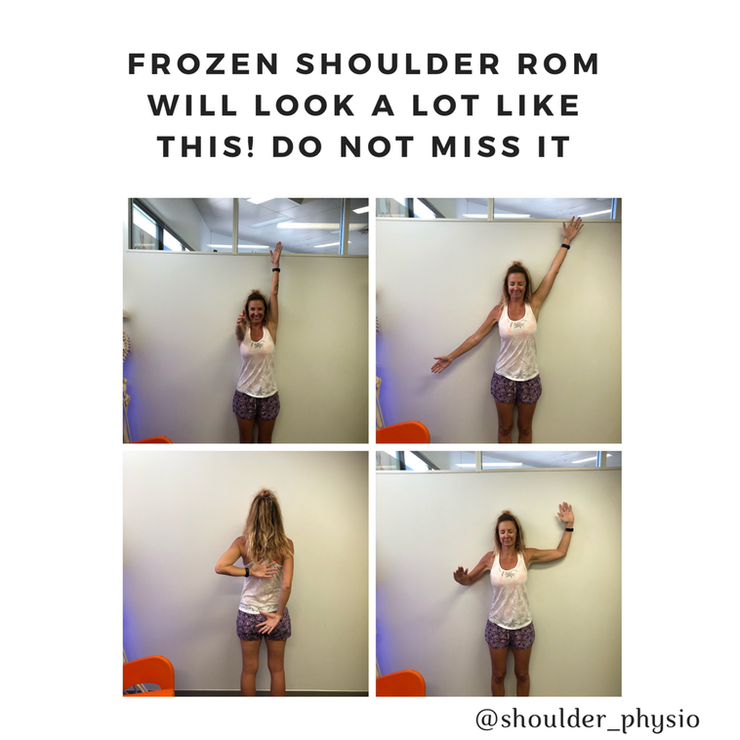
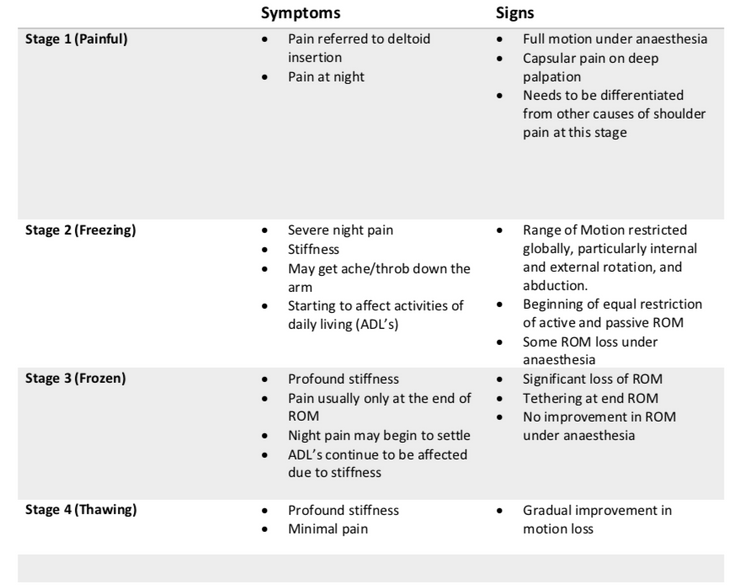
Despite the uncertainty pertaining to the patho-aetiology, there is some consensus regarding the progression of the condition. A progressive loss of mobility of the shoulder with associated pain and disability. The condition has classically been categorized in 4 stages; painful, freezing, frozen, and thawing (see table below) (5). However, since these stages can overlap, a more useful categorization may be pain greater than stiffness or stiffness greater than pain (3,6). This simplified method of organization may also help stage management.
The incidence of FS is cited as being between 3-5% in the general population. However the true incidence may be less than this. The incidence of FS appears to be considerably higher in people with diabetes, where figures of up to 30% have been reported (7). There may also be an association with hypothyroidism (8), and there also appears to be a high incidence of Dupuytrens contracture in people with FS (9,10) and both Dupuytrens contracture and FS are common in people with diabetes (11). FS may slightly be more common in women than men and tends to affect those between the ages of 40 to 60 (12). Recurrence of FS on the same side appears to be unusual, and there has been documented cases involving the contralateral shoulder, ranging from 6-34% (12).
FS is generally classified into 1) primary idiopathic and 2) secondary FS. Primary idiopathic FS includes those without a main inciting event leading to the onset of symptoms. Secondary FS can be attributed to some causative event and is further sub-categorized into intrinsic (e.g. rotator cuff pathology), extrinsic (e.g. clavicle fracture or breast surgery), and systemic (e.g. diabetes or hypothyroidism) (13).
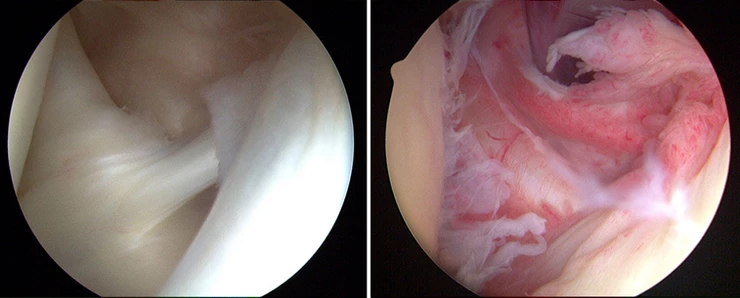
The anatomical structures that have been found to be pathological in FS most often are a thickened coraco-humeral ligament, thickening of the joint capsule in the rotator interval and axillary recess, thickening of the synovial membrane in the rotator interval and axillary recess, a distended bursa within the superior subscapularis recess and tenosynovitis of the long head of biceps tendon (4). Histological samples of the capsule have revealed a high population of fibroblasts and contractile myofibroblasts, a fibrotic process limited to the anterior part of the capsule and elevated inflammatory cytokines in the subacromial bursa and anterior capsule (4). These findings have lead Tamai et al 2014 to hypothesize that an immunological event could lead to inflammatory synovitis causing anterosuperior capsular fibrosis that results in the classic stiffness and pain associated with FS (15).
Subjective examination
The natural history of FS is somewhat controversial. The consensus is generally that FS is a self-limiting condition that resolves gradually over 2-3 years (16). However, it appears many people experience ongoing persistent deficits in ROM and the presence of pain many years after the onset of symptoms (17, 18). Hand et al 2008 reported that after 4 years 41% of individuals were still experiencing symptoms related to FS and Shaffer 1992 reported that 50% of people with FS still had symptoms on average 7 years after diagnosis (19,20). A recent systematic review by Wong et al 2017 found a lack of evidence to support the theory that FS progresses neatly though time defined stages until full resolution of symptoms occurs without any treatment (17).
Subjectively, those experiencing primary idiopathic FS will often report a painful shoulder that progressively becomes stiff. Typically, the continuum of FS begins with pain followed by stiffness (21). The location of the pain is usually the deltoid tuberosity and more diffusely around the shoulder girdle (16), although the pain can radiate and throb down the arm. Pain type is usually a constant ache that can become sharp with fast or jolting movements (22). Sleep is often affected in the painful and freezing stage, possibly due to an active synovitis process (22). Activities of daily living will become difficult secondary to both pain and stiffness and will usually affect grooming and dressing activities and reaching overhead and behind the back (23).
Russell et al 2014 conducted a study comparing group exercise supervised by a physiotherapist (group 1) Vs individual multimodal physiotherapy (group 2) versus independent home exercise (group 3) in the effectiveness of conservatively managing FS (24). It was found that both physiotherapy interventions (groups 1&2) were more effective than individual home exercise, and that group exercise (group 1) resulted in the best overall patient-reported outcomes (24). It was hypothesized that the group nature of the intervention provided a clinical setting where people with FS could talk to each other and experience peer support and also derive motivation to continue to progress their rehabilitation (24). The importance of self-efficacy was also promoted and Chester et al 2016 reported that low pain self-efficacy can predict a worse outcome from shoulder pain (25). In addition, both physiotherapy groups in the Russell et al 2014 study were associated with a reduction in anxiety symptoms and it was found that anxiety and depression are strongly correlated with symptoms in this particular FS cohort (24). Pain, depression and anxiety are often co-morbid symptoms that appear together in a bi-directional manner (26). As such it is a key finding that a group-based exercise class led by a physiotherapist may help reduce the stress and anxiety associated with the protracted symptoms of this condition, which, in turn, may help reduce the pain and disability associated with FS and improve the cost effectiveness of its management (24).Due to the chronicity associated with FS, it is worth considering common psychological symptoms that may appear with persistent pain in addition to physical symptoms. When an individual is experiencing persistent pain, a clinician shoulder consider:
- Lifestyle factors (sleep, physical activity, diet etc.)
- Psychological factors (fear, stress, depression etc.)
- Cognitive beliefs (personal beliefs about injury)
- Individual factors (personal experience)
All of these factors can influence the perception of pain (27).There are a number of strategies to address these factors, including pain education, cognitive behavioural therapy, exposure therapy, meditation and more.If a clinician is not confident or competent in dealing with psychosocial elements of pain, then a timely referral to another member of the multi-disciplinary team, such as a psychologist is warranted.
There are several validated outcome measures that are used to assess patients with shoulder pain. The most widely used in FS are the Constant score (28), the Disability of the Arm, Shoulder and Hand (DASH) (29), the Shoulder Pain and Disability Index (SPADI) (30), the American Shoulder and Elbow Surgeons (ASES) (31), and the Simple Shoulder Test (SST). The ASES, SPADI, DASH and SST have been shown to be reliable, valid, and responsive across a number of shoulder pathologies, including FS (32). Although there is no current definitive ‘gold standard’ outcome measurement that may be recommended for clinical practice or research (33), Roy et al 2009 recommends the DASH as the preferred outcome measure when assessing emotional and social function, in addition to pain and physical function (32). Standardizing outcome measures across clinical trials would facilitate a greater understanding of the effectiveness of interventions investigated for this condition.
The next review will be Frozen Shoulder instalment 2. This will look at objective examination and differential diagnosis.
Try and contain your excitement.
NOTE: If still struggling with frozen shoulder in the clinic, this is a special interest of mine and will be covered in depth in my shoulder course. Link below:
https://www.eventbrite.com.au/e/shoulder-physio-workshop-tickets-56021690384
References
-
Codman E. The shoulder: Rupture of the supraspinatus tendon and other lesions in or about the subacromial bursa. Boston: Thomas Todd Company; 1934.
-
Neviaser, JS. Adhesive capsulitis of the shoulder. Journal of Bone and Joint Surgery America (1945) 27(2): 211-222
-
Lewis, J. Frozen shoulder contracture syndrome – Aetiology, diagnosis, and management. Manual Therapy 20 (2015) 2-9.
-
Ryan V, Brown H, Minns Lowe CJ, Lewis JS. The pathophysiology associated with primary (idiopathic) frozen shoulder: A systematic review. BMC musculoskeletal disorders. 2016;17(1):340.
-
Neviaser, AS., Hannafin, JA. Adhesive capsulitis. A review of current treatment. Clinical sports medicine update (2010).
-
Hanchard, N., Goodchild, L., Thompson, J. Evidence based clinical guidelines for the diagnosis, assessment, and physiotherapy management of contracted (frozen) shoulder. Standard physiotherapy (2011).
-
Whelton, C., Peach, CA. Review of diabetic frozen shoulder. European journal of orthopaedic surgery and traumatology (2017).
-
Schiefer, M., Santos Teixeria, PF., Fontonelle, C., Carminatti, T., Santos, DA., Righi, LD., Conceicao, FL. Prevalence of hypothyroidism in patients with frozen shoulder. Journal of shoulder and elbow surgery (2017).
-
Smith SP, Devaraj VS, Bunker TD. The association between frozen shoulder and Dupuytren's disease. J Shoulder Elb Surg 2001;10:149e51.
-
Degreef I, Steeno P, De Smet L. A survey of clinical manifestations and risk factors in women with Dupuytren's disease. Acta Orthop Belg 2008;74:456e60.
-
Smith CD, White WJ, Bunker TD. The associations of frozen shoulder in patients requiring arthroscopic release. Shoulder & Elb 2012;4:87e9.
-
Dawson, J., Shepperd, S., Carr, A. An overview of factors relevant to undertaking research and reviews on the effectiveness of treatment for frozen shoulder. Shoulder and elbow (2010).
-
Zuckerman, JD., Rokito. Frozen shoulder: a consensus definition. Journal of shoulder and elbow surgery (2011).
-
Xu Y, Bonar F, Murrell GA, et al. Enhanced expression of neuronal proteins in idiopathic frozen shoulder. J Shoulder Elbow Surgery. 2012;21(10):1391–7. doi:10.1016/j.jse.2011.08.046.
-
Tamai, K., Akutsu, M., Yano, Y. Primary frozen shoulder: brief review of pathology and imaging abnormalities. Journal of orthopaedic science (2014).
-
Guyver, PM., Bruce, DJ., Rees, JL. Frozen shoulder – A stiff problem that requires a flexible approach. Maturitas (2014).
-
Wong, CK., Levine, WN., Deo, K., Kesting, RS., Mercer, EA., Schram, GA., Strang, BL. Natural history of frozen shoulder: fact or fiction? A systematic review. Physiotherapy (2017).
-
Favejee, MM., Huisstede, BMA., Koes, BW. Frozen shoulder: the effectiveness of conservative and surgical interventions – systematic review. British journal of sports medicine (2010).
-
Hand, C., Clipsham, K., Rees, JL., Carr, AJ. Log-term outcome of frozen shoulder. Journal of shoulder and elbow surgery (2008).
-
Shaffer, B., Tibone, JE., Kerlan, RK. Frozen shoulder, a long term follow-up. Journal of bone and joint surgery (1992).
-
Le, HV., Lee, SJ., Nazarian, A., Rodriguez, EK. Adhesive capsulitis of the shoulder: review of pathophysiology and current clinical treatments. Shoulder and elbow (2017).
-
Struyf, F., Meeus, M. Current evidence on physical therapy in patients with adhesive capsulitis: what are we missing? Clinical Rheumatology (2014) 33: 593-600.
-
Kelley, MJ., Shaffer, MA., Kuhn, JE., Michener, LA., Seitz, AL., Uhl, TL., Godges, JJ., McClure, PW. Shoulder pain and mobility deficits: Adhesive capsulitis. Clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American physical therapy association. Journal of orthopaedics and sports physical therapy (2013).
-
Russell, S., Jariwala, A., Conlon, R., Selfe, J., Richards, J., Walton, M. A blinded, randomised, controlled trial assessing conservative management strategies for frozen shoulder. Journal of shoulder and elbow surgery (2013).
-
Chester, R., Jerosch-Herold, C., Lewis, J., Shepstone, L. Psychological factors are associated with the outcome of physiotherapy for people with shoulder pain: a multicentre longitudinal cohort study. British Journal of Sports Medicine (2018).
-
De Heer, EW., Gerrits, MMJG., Beekman, ATF., Dekker, J., van Marwijk, HWJ,.de Waal, MWM., Spinhoven, P., Penninx, BWJH., van der Feltz-Cornelius, CM. The Association of Depression and Anxiety with Pain: A Study from NESDA. PLOS (2014).
-
Simons, LE., Elman, I., Borsook, D. Psychological processing in chronic pain: A Neural Systems Approach. Neuroscience and Biobehavioural Reviews (2014).
-
Constant, CR., Murley, AH. A clinical method of functional assessment of the shoulder. Clinical orthopaedics and related research (1987).
-
Hudak PL, Amadio PC, Bombardier C. Development of an upper ex- tremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29:602-608. http://dx.doi.org/10.1002/ (SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L
-
Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y. Develop- ment of a shoulder pain and disability index. Arthritis Care Res. 1991;4:143-149.
-
Richards RR, An KN, Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347- 352. http://dx.doi.org/10.1016/S1058-2746(09)80019-0
-
Roy, JS., MacDermaid, JC., Woodhouse, LF. Measuring Shoulder Function: A systematic Review of Four Questionnaires. Arthritis Care and Research (2009).
Ready to gain the confidence to manage any shoulder pain patient who comes to see you?
My comprehensive course – developed over 10 years of treating shoulder patients and researching and educating professionals about shoulder joint function – covers all the above areas and more. In over 16 hours of training delivered in an engaging, self-paced, online format, you’ll learn everything you need to know to feel at ease treating people with shoulder pain.


