Literature Review February 2019 - CSAW
Feb 12, 2019
Shoulder Physio Literature Review
#1 February 2019
Welcome to the inaugural Shoulder Physio literature review. I will release the reviews monthly and intend to succinctly summarise important scientific journal articles that have the potential to inform, modify or progress how we manage shoulder pain. Enjoy.
Introduction
The first piece of literature up for review is the now infamous CSAW (Can Shoulder Arthroscopy Work) study. Published by Beard et al 2018 in the prestigious Lancet journal (https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(17)32457-1/fulltext).
The aims of the study were to compare subacromial decompression surgery for shoulder "impingement" to a sham surgery where the "essential" decompression component of the surgery wasn't performed. A secondary aim was to compare surgical intervention (decompression or sham) to no treatment. Participants were followed up at 6 and 12 months post intervention.
Background information
So why conduct this seemingly extreme study in the first place? The past 5-10 years has seen increasing uncertainty surrounding subacromial impingement as a diagnosis and also a patho-aetiological process. Simply put, we have no idea whether external impingement of the acromion on the underlying rotator cuff and bursa is the cause of the classic signs and symptoms associated with rotator cuff related shoulder pain. These signs and symptoms include:
- Pain with shoulder abduction between 70-120 degrees (painful arc)
- Pain with impingement special orthopaedic tests, such as Hawkins-Kennedy and Neer's tests
- Pain with resisted external/internal rotation of the shoulder
The term impingement was put forward by Charles Neer in 1972 who reported impingement of the cuff against the undersurface of the acromion accounted for 95% of rotator cuff pathology (I like the confidence). As a result, the past 40 years have seen "all" musculoskeletal practitioners obsess about the acromion and how the cuff must never come into contact with it (without it becoming shredded!).
This led to large increases in subacromial decompression surgeries around the world (multi-billion dollar annual industry in the USA) and physio's, chiro's and osteo's doing their utmost to centralise the humeral head on the glenoid to avoid superior translation in the direction of the demonic acromion. So we started to obsess about "postural imbalances" and scapula kinematics and tightness of shoulder muscles etc which were supposed to have a large influence on the subacromial space and therefore predispose to pain. Pectoral, posterior cuff and latissimus dorsi stretching became the in vogue thing to do. As did, scapular stability work and low grade rotator cuff rotation strength work with those therabands. We were to avoid movements that impinge the rotator cuff (exercises such as the upright row) if we wanted to have good shoulder health. We were taught and continue to teach the subacromial bursa is the important pain generating structure in the shoulder and it should be injected with a corticosteroid to diminish its output. Whilst the SAB certainly IS nociceptive, we must figure out why it has become painful and not merely treat the symptoms. Pain is an emergent and multi-factorial experience and often cannot be attributed entirely to a single structure.
Then, controversially, we started to see that some people with a problematic acromion actually don't always develop pain. We also observed people with a perfect acromion going on to develop pain. We found that structure often correlates poorly with symptoms. For more on this read Jeremy Lewis (https://www.sciencedirect.com/science/article/abs/pii/S1356689X16000400). Ketola et al 2013 then ran a great study that compared surgery to exercise therapy for subacromial impingement and found no differences between the 2 groups after 5 years (https://www.ncbi.nlm.nih.gov/pubmed/23836479). This raised suspicion of how important the acromion was and implicated more the strength and robustness of the rotator cuff tendons and how they respond to mechanical load. Similar to other tendinopathies in the body, right! (think achilles and patella).
Which leads us to CSAW
CSAW used a multicentre, randomised, pragmatic, parallel group, placebo-controlled, 3 group trial. In other words, a fairly thorough study.
3 groups were:
-
Subacromial decompression surgery (n=106)
-
Placebo/sham surgery (n=103)
-
No treatment (n=104)
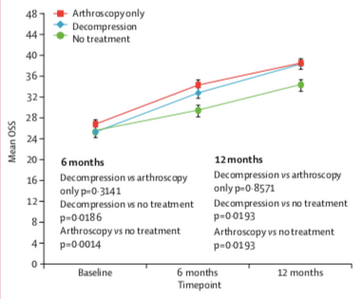
Follow up was recorded at 6 and 12 months. The main outcome measure was the Oxford Shoulder Score.
Results
There were no differences between each surgical group at any stage of follow up (real Vs sham surgery). Both surgical groups performed better than no treatment.
Interpretation
Both surgical groups improved significantly and in alignment with each other. BUT there were no differences between the 2 groups. So what is the mechanism of action if sham surgery is performed equally to surgical decompression? Intellectually, it is probably due to contextual and psychological factors. We know the power that expectations have on patient outcomes as pointed out by Chester et al 2018 (https://bjsm.bmj.com/content/52/4/269.short). If somebody expects to get better with a certain intervention, they most probably will. This works equally in the opposite direction where negative expectations result in worse outcomes. We also can't discount the effect of post-operative rehab/physiotherapy where a concerted period of strength and conditioning was undertaken by both surgical groups. There was also a period of relative unloading in both groups, which can reduce pain associated with reactive tendinopathy. Additionally, a person may have more compliance or investment in their rehab after surgery and complete their exercises more diligently whereas this may not have been the case prior to surgery. This is especially true if a person with "impingement" is convinced their issue is coming from a bone impinging on a tendon - how can this be helped with physiotherapy? Immediately their expectations are that surgery will likely be the end result and are simply going through the motions of conservative rehab to satisfy the surgeon and GP prior to escalating management to surgery. Cuff and Littlewood 2017 have written an excellent article on this (https://www.ncbi.nlm.nih.gov/pubmed/29065348). This has a huge influence on patient outcomes and the onus is on all of us to provide thorough and tailored education to align patient expectations with current scientific literature. If this is neglected or not prioritised we are simply wasting our time trying to manage people who have poor expectations on the effectiveness of physiotherapy.
Both surgical groups were statistically better than no treatment, although clinically there wasn't a large difference between them. Ideally, a 4th group who engaged in an exercise therapy regime aimed at progressively loading the shoulder would have been included. Lucky this WAS included in a recent study by Paavola et al 2018 (https://www.bmj.com/content/362/bmj.k2860). To be discussed in the future.
Final word (bias alert)
It seems quite clear from the available evidence that sham and actual surgery for subacromial impingement are NO DIFFERENT in patient reported outcomes. Although no long-term studies have been performed. This study is a gigantic leap forward in exploring the mechanism behind the effectiveness of arthroscopy for rotator cuff related shoulder pain.
The results of CSAW raise real concerns about the term impingement. How could sham surgery be effective when the impinging structures are still in situ? Maybe there is more to it (who would have thought). It also may implicate an intrinsic tendon failure/irritation secondary to acute overload or a traumatic incident as seen in other tendinopathies. It also highlights the importance of contextual and psychological factors such as patient expectations, beliefs, and past experiences in the human pain experience.
As MSK practitioners we need to consider the whole human being when trying to determine what is driving their pain experience. We must move beyond prioritising biological and mechanical factors in people with pain and consider all phenomena capable of influencing pain. Although, biological factors DO matter. Let's not get too tribal here - bio psychosocial - it all matters.
I have neglected to delve into the economic impact of this highly expensive surgical procedure, as I am not an economist. BUT, I think we can clearly see of the mechanism of action is mostly placebo and post-operative rehabilitation, we are wasting millions of dollars on surgical costs when these precious $$ could be best used elsewhere. Food for thought.
As a final word, I am not against surgery for rotator cuff related shoulder pain, I just think it should be a last resort. It should only be considered after failure of an appropriate and individualised progressive resistance based exercise regime that is given at least 12 weeks to have an affect. If surgery is performed before this, based on the available evidence, it is likely not in the best interests of the patient.
The Complete Clinician
Tired of continuing education that treats clinicians like children who can’t think for themselves?
The Complete Clinician was built for those who want more.
It’s not another lecture library, it’s a problem-solving community for MSK professionals who want to reason better, think deeper, and translate evidence into practice.
Weekly research reviews, monthly PhD-level lectures, daily discussion, and structured learning modules to sharpen your clinical edge.
Join the clinicians who refuse to be average.


